Claims Analytics Use Case
Auto Insights can help insurance teams automate claims performance analysis, drill into claims trends, and spot anomalous claim rates.
This article covers:
Example insights from this use case.
Recommended data structure for this use case.
What Sort of Insights Can Auto Insights Help Me Uncover?
We've outlined some example questions that Auto Insights can help answer through a combination of its proactive insights, Missions, and What caused this? analysis.
Automate claims performance analysis:
Number of Claims by Department
Average Time to Payment by Agent
Number of Claims by Policy Type
Drill into claims trends:
Trend of Claims by Claim Reason in Sydney
Seasonality of Claims
Compare Claim Amounts for Theft in Metropolitan and Regional areas
Average Time to Close Claims by Department and Claim Type
Spot anomalous claim rates:
Average Number of Claims per customer
Claim Amount by Claim Reason in Sydney
Top 20 Claims by Claim Amount and Claim Reason last quarter
How Do I Structure My Data?
Auto Insights requires structured, transactional data, with at least 1 measure (for example, Number of Claims) and 5 segments (for example, Claim Type). In addition, we recommend at least 7 months of data (at monthly or daily granularity) so you can take full advantage of Auto Insights' Unexpected Changes feature.
Example Data Structure
Please click on the picture to download a larger copy of the image.
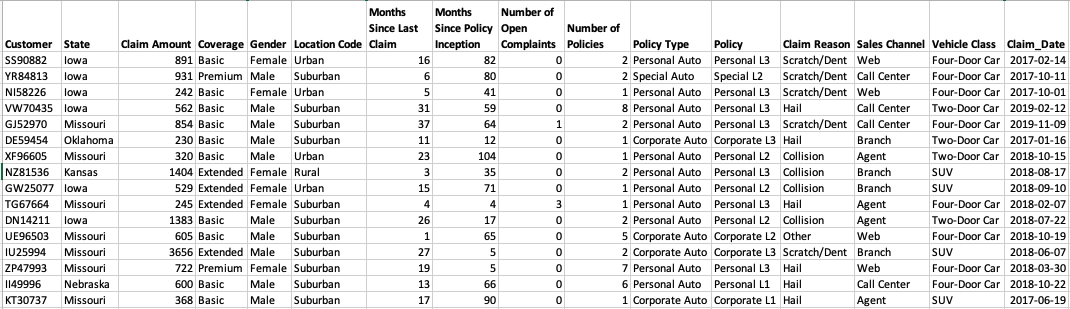
Please refer to Dataset Requirements for more information about data structure.
Segments
Here are some of the typical segments we find in revenue data. A segment is a qualitative value, like names or categories:
Claim attributes: Claim reason, Claim type, Team, Department
Policy attributes: Policy type, Policy name, Months since last claim, Agent assigned, claim channel, coverage type
Claimant attributes: Age, Gender, Location, etc.
Measures
A measure is a quantitative, numeric value. Some of the typical measures include customer ID, number of claims, claim amount, time to close claims, and time to payment.